Hospice Care: How To Use The Palliative Performance Scale
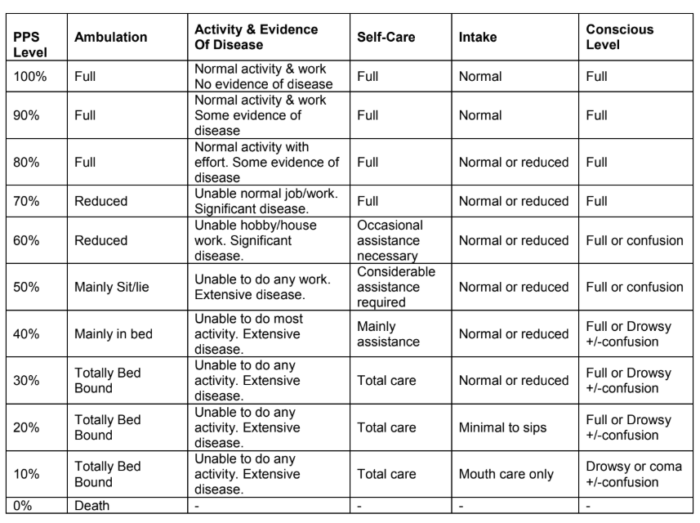
The Palliative Performance Scale (PPS) is a validated and reliable tool used to assess a patient’s functional performance and to determine progression toward end of life. However, it does not take the place of a physician’s professional judgment.
How to use the Palliative Performance Scale
1. PPS scores are determined by reading horizontally at each level to find a “best fit” for the patient who is then assigned the PPS% score.
2. Begin at the left column and read downwards until the appropriate ambulation level is reached, then read across to the next column and downwards again until the activity/evidence of disease is located. These steps are repeated until all five columns are covered before assigning the actual PPS for that patient. In this way, “leftward” columns (columns to the left of any specific column) are “stronger” determinants and generally take precedence over others.
Example 1: A patient who spends the majority of the day sitting or lying down due to fatigue from advanced disease and requires considerable assistance to walk even for short distances but who is otherwise fully conscious level with good intake would be scored at PPS 50%.
Example 2: A patient who has become paralyzed and quadriplegic requiring total care would be PPS 30%. Although this patient may be placed in a wheelchair (and perhaps seem initially to be at 50%), the score is 30% because he or she would be otherwise totally bed bound due to the disease or complication if it were not for caregivers providing total care including lift/transfer. The patient may have normal intake and full conscious.
Example 3: However, if the patient in example 2 was paraplegic and bed bound but still able to do some self-care such as feed themselves, then the PPS would be higher at 40 or 50% since he or she is not “total care.”

CONTINUA LEARNING
Simplify Your Hospice Team’s Training and Skill Building
A complete solution for your agency: more than 125 hospice courses, caregiver in-services, training plans, and more.
3. PPS scores are in 10% increments only. Sometimes, there are several columns easily placed at one level but one or two which seem better at a higher or lower level. One then needs to make a “best fit” decision. Choosing a “half-fit” value of PPS 45%, for example, is not correct. The combination of clinical judgment and “leftward precedence” is used to determine whether 40% or 50% is the more accurate score for that patient.
4. PPS may be used for several purposes. First, it is an excellent communication tool for quickly describing a patient’s current functional level. Second, it may have value in criteria for workload assessment or other measurements and comparisons. Finally, it appears to have prognostic value.

Definition of Terms for Palliative Performance Scale in Hospice Care
As noted below, some of the terms have similar meanings with the differences being more readily apparent as one reads horizontally across each row to find an overall “best fit” using all five columns.
Ambulation
The items mainly sit/lie, mainly in bed and totally bed bound are clearly similar. The subtle differences are related to items in the self-care column. For example, totally bed bound at PPS 30% is due to either profound weakness or paralysis such that the patient not only can’t get out of bed but is also unable to do any self-care. The difference between sit/lie and bed is proportionate to the amount of time the patient is able to sit up vs need to lie down.
Reduced ambulation is located at the PPS 70% and PPS 60% level. By using the adjacent column, the reduction of ambulation is tied to inability to carry out their normal job, work occupation or some hobbies or housework activities. The person is still able to walk and transfer on their own but at PPS 60% needs occasional assistance.
Activity & Extent of Disease
Some, significant and extensive diseases refer to physical and investigative evidence which shows degrees of progression. For example in breast cancer, a local recurrence would imply “some” disease, one of two metastases in the lung or bone would imply “significant” disease, whereas multiple metastases in lung, bone, liver, brain, hypercalcemia or other major complications would be “extensive” disease. The extent may also refer to progression of disease despite active treatments. Using PPS in AIDS, “some” may mean the shift from HIV to AIDS, “significant “ implies progression in physical decline, new or difficult symptoms and laboratory findings with low counts. “Extensive” refers to one or more serious complications with or without continuation of active antiretroviral, antibiotics, etc.
The above extent or disease is also judged in context with the ability to maintain one’s work and hobbies or activities. Decline in activity may mean the person still plays golf but reduces from playing 18 holes to 9 holes, or just a par 3, or to backyard putting. People who enjoy walking will gradually reduce the distance covered, although they may continue trying, sometimes even close to death (e.g. trying to walk the halls).
Self-Care
Occasional assistance means that most of the time patients are able to transfer out of bed, walk, wash, toilet and eat by their own means, but that on occasion (perhaps once daily or a few times weekly) they require minor assistance.
Considerable assistance means that regularly every day the patient needs help, usually by one person, to do some of the activities noted above. For example, the person needs help to get to the bathroom but is then able to brush his or her teeth or wash at least hands and face. Food will often need to be cut into edible sizes but the patient is then able to eat of his or her own accord.
Mainly assistance is a further extension of “considerable”. Using the above example, the patient now needs help getting up but also needs assistance washing his face and shaving, but can usually eat with minimal or no help. This may fluctuate according to fatigue during the day.
Total care means that the patient is completely unable to eat without help, toilet or do any self-care. Depending on the clinical situation, the patient may or may not be able to chew and swallow food once prepared and fed to him or her.
Intake
Changes in intake are quite obvious with normal intake referring to the person’s usual eating habits while healthy. Reduced means any reduction from that and is highly variable according to the unique circumstances. Minimal refers to every small amounts, usually pureed or liquid, which are well below nutritional sustenance.
Conscious Level
Full consciousness implies full alertness and orientation with good cognitive abilities in various domains of thinking, memory, etc.
Confusion is used to denote presence of either delirium or dementia and is a reduced level of consciousness. It may be mild, moderate or severe with multiple possible etiologies.
Drowsiness implies fatigue, drug side effects, delirium or closeness to death and is sometimes included in the term stupor.
Coma in this context is the absence of response to verbal or physical stimuli; some reflexes may or may not remain. The depth of coma may fluctuate throughout a 24 hour period.
Palliative Performance Scale (PPSv2)
Version 2
© Copyright Notice.
The Palliative Performance Scale version 2 (PPSv2) tool is copyrighted to Victoria Hospice Society and replaced the first PPS published in 1996 [J Pall Care 9(4): 26-32]. It cannot be altered or used in any way other than as intended and described here. Programs may use PPSv2 with appropriate recognition. Correspondence should be sent to Medical Director, Victoria Hospice Society, 1900 Fort St. Victoria, BC, V8R1J8, Canada.
If you found this article informative and useful share it with your friends and colleagues.
