Transform Care, Boost Staff Retention, Automate Home Care Training
Built for home health care training online, Continua Learning is the mobile solution for achieving compliance, training staff on the go, and easily tracking it all from one place.

Trusted by leaders in home care and home health
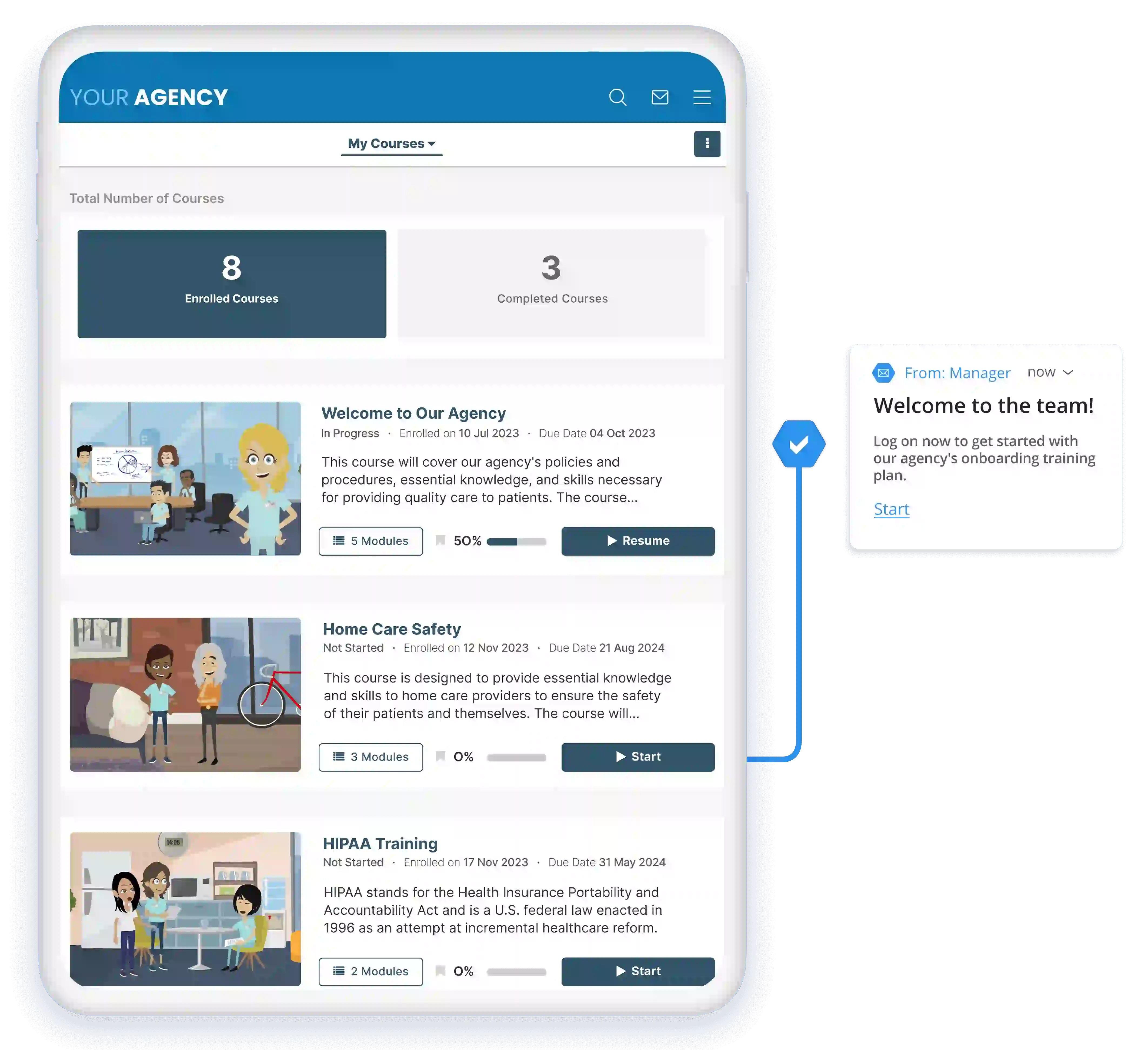

Onboarding Software for Home Care and Home Health Agencies
Onboarding New Staff
Create onboarding training plans that combine your agency's training with our courses for a complete program. Dynamically enroll your learners based on their unique job roles on day one.
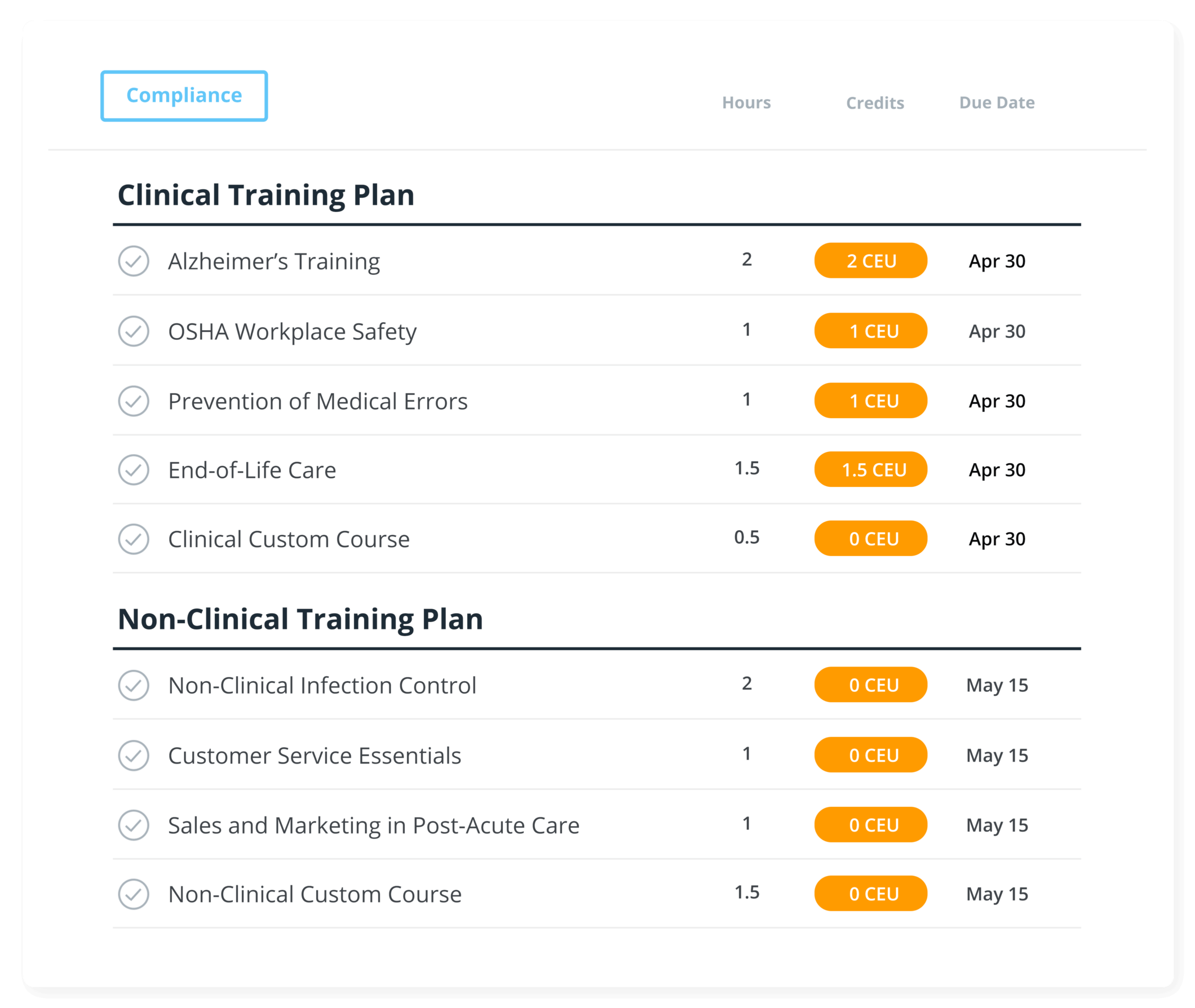
Annual Compliance
We help you build your agency's annual compliance training plans that target clinical, non-clinical, HHA, caregiver, and more. Assign due dates and easily track your team's progress with status reports.
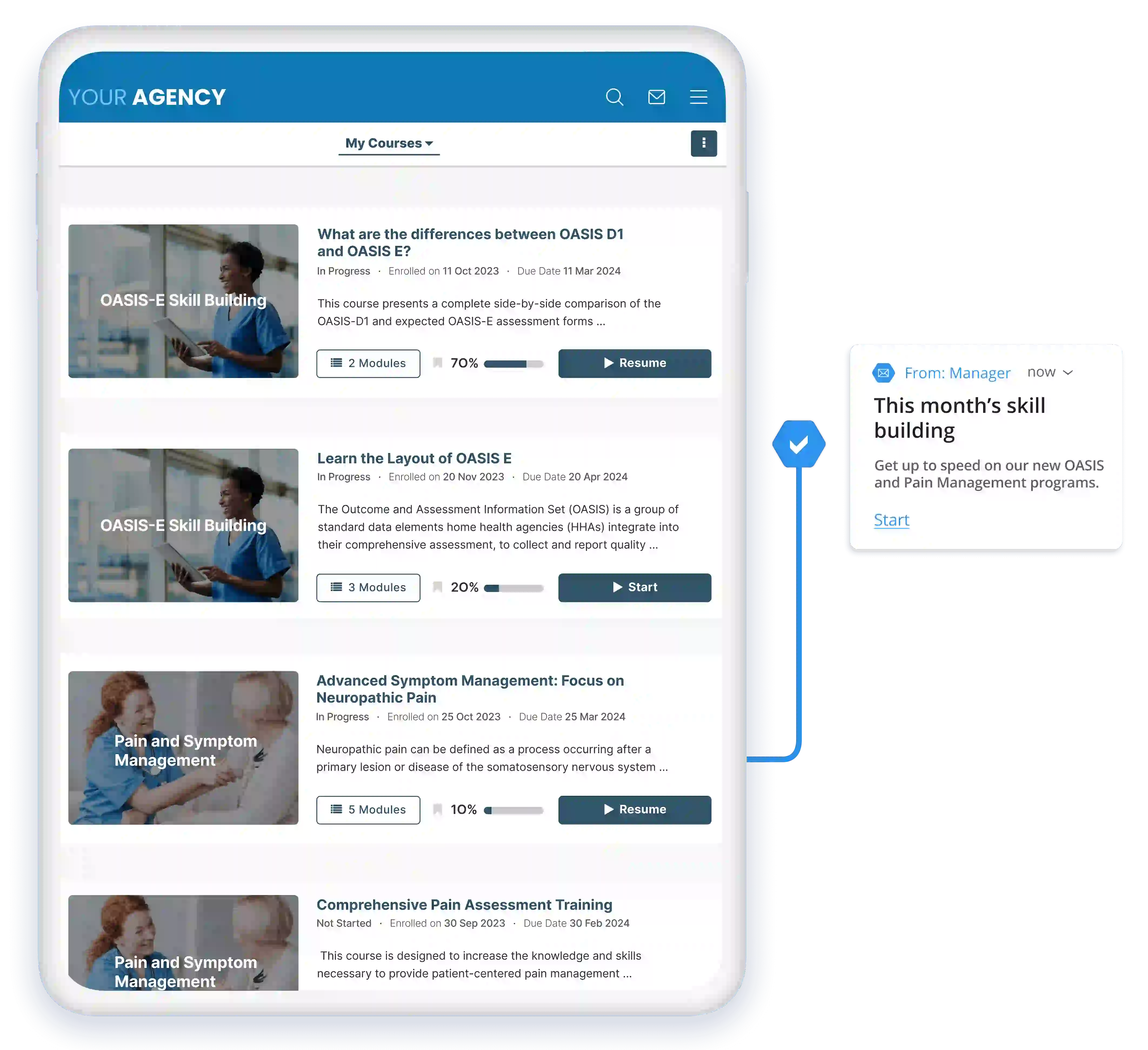
Skill Building
Target gaps in your staff's performance, new regulations, and industry changes with skill-building learning paths. Libraries include coding, OASIS, leader/manager, marketing, clinical skills, and many more.
Continuing Education
Your clinical staff will get unlimited access to over 500 CEUs to help meet their license and annual continuing education requirements.
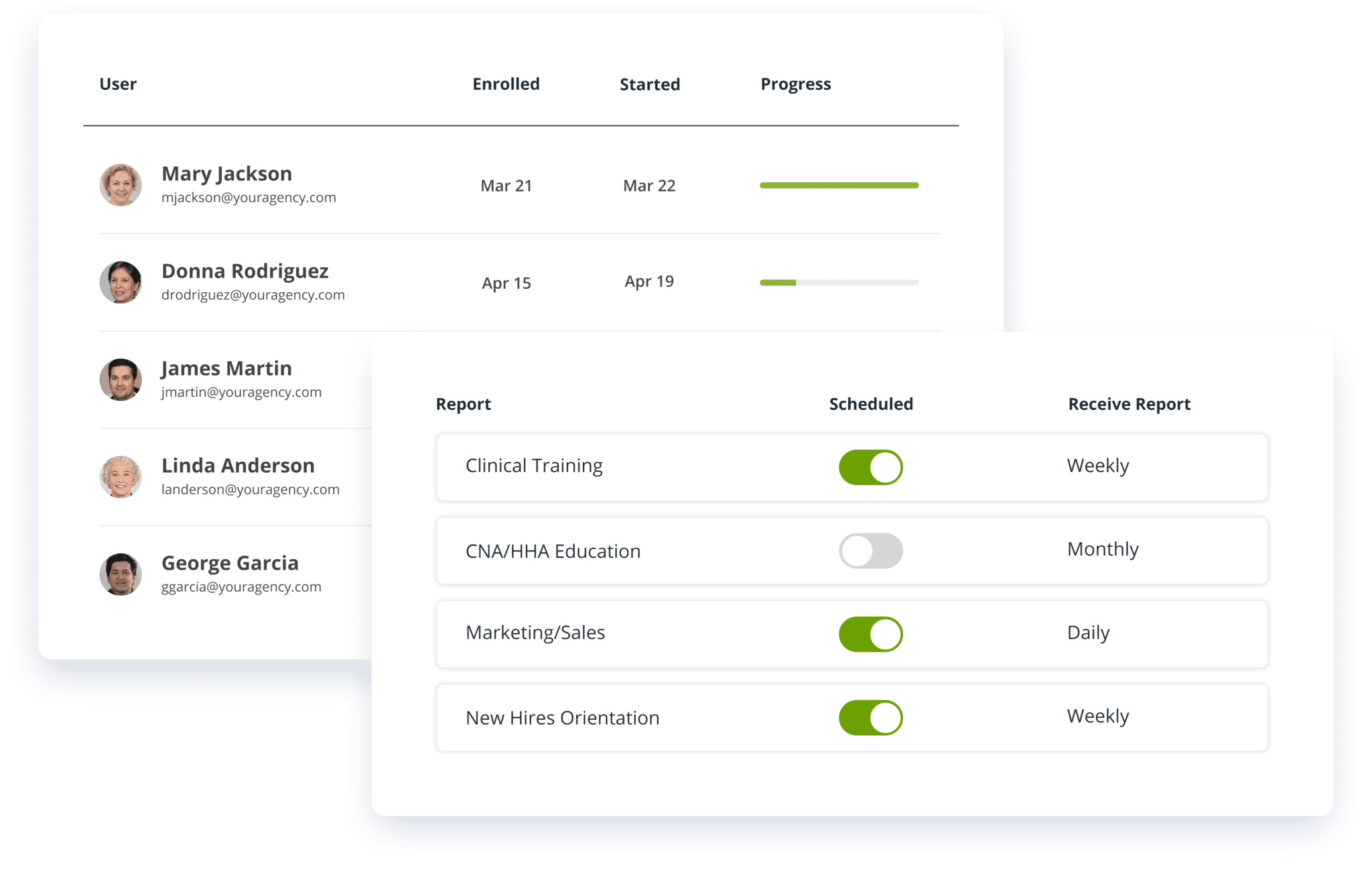
Manage, Track, and Report
Assign, track, and record online, ILT and external training - all from one place - and use automated weekly reports for managers to take the guesswork out of compliance.
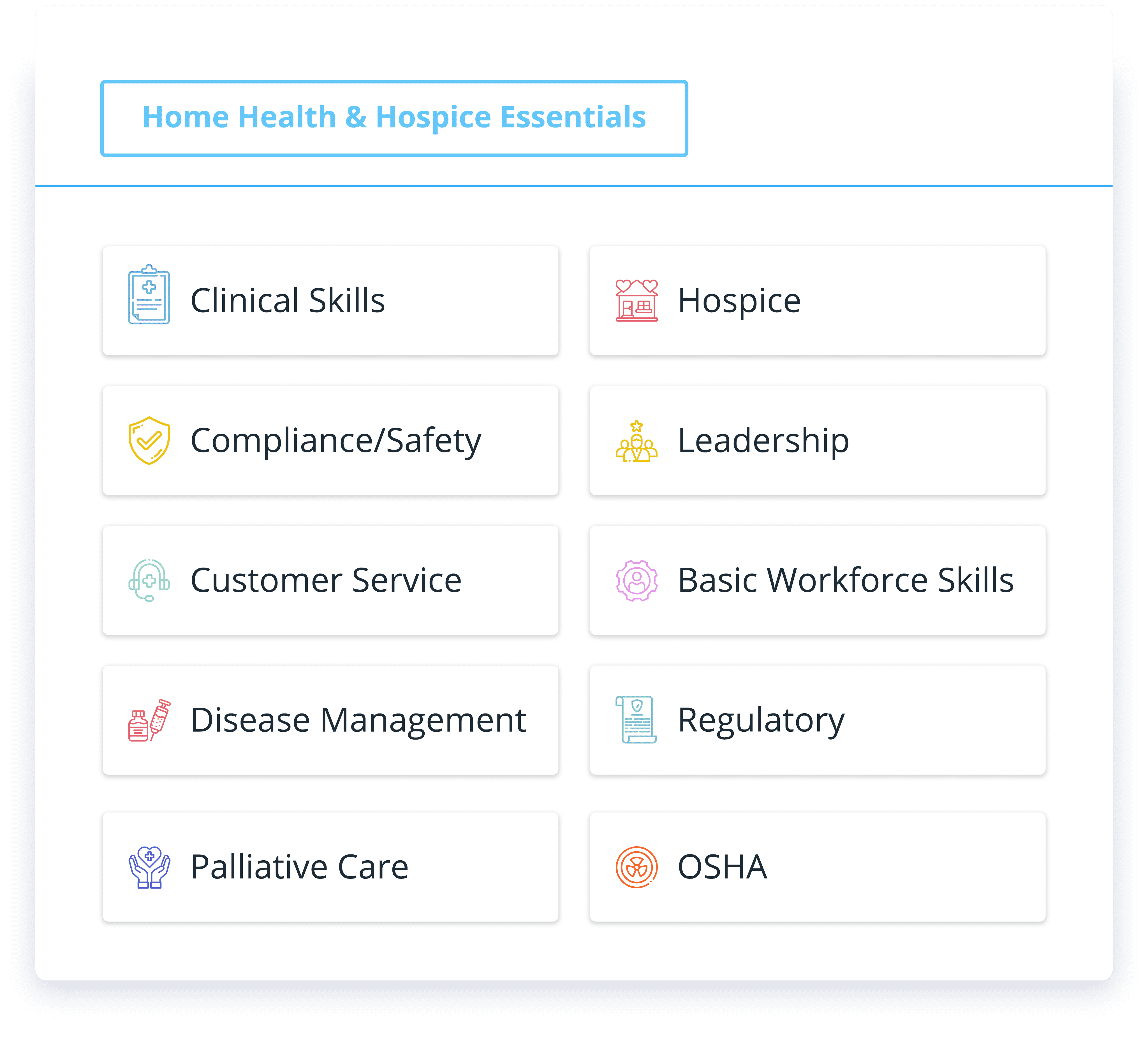
CONTINUA LEARNING COURSE LIBRARY
Home care and home health compliance training
Get unlimited access to over 350 courses and 500+ CEUs that cover all your training needs: coding, OASIS, home health, hospice, caregiver in-services, leader/manager, marketing, clinical skills, annual requirements, and more.
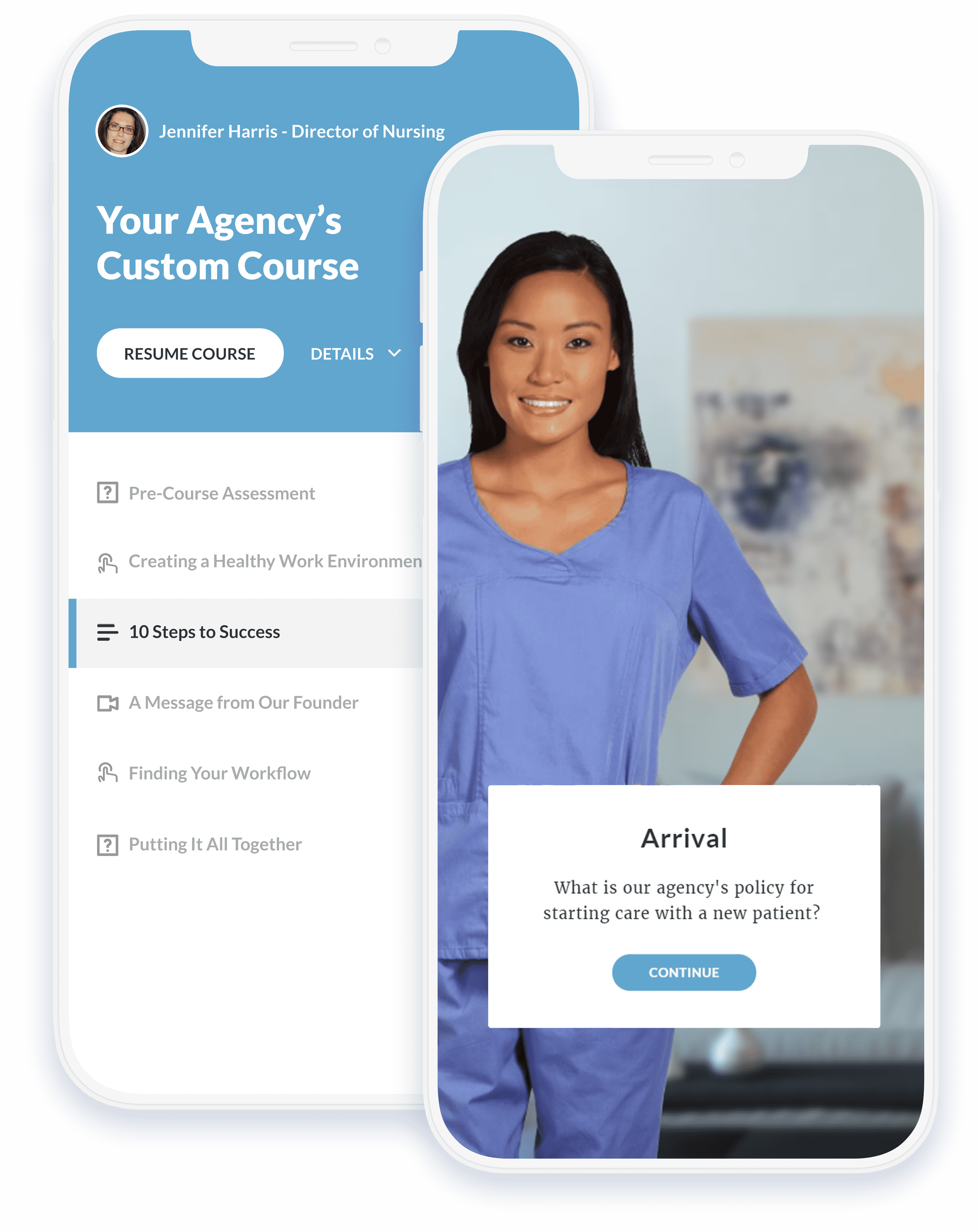
CUSTOM COURSE CREATION
Your content, transformed into mobile training
Your unique care techniques are what set you apart from the rest. Combine your training with our courses for a complete training experience.
Unlike other services, we do the heavy lifting. Send us your educational material, and our instructional designers will turn it into mobile-ready eLearning - at no extra cost.
Perfect for large and mid-sized home care and home health agencies
"Continua has been a great partner in our efforts to develop customized training for our staff. Our staff has completed thousands of courses offered through Continua since the inception of our relationship. Monitoring and reporting progress is simple and easy, and our staff finds the platform user-friendly. There has always been a friendly, customer-focused feel to our relationship."
 Chris Chimenti, Senior Director, HCR Home Care
Chris Chimenti, Senior Director, HCR Home Care
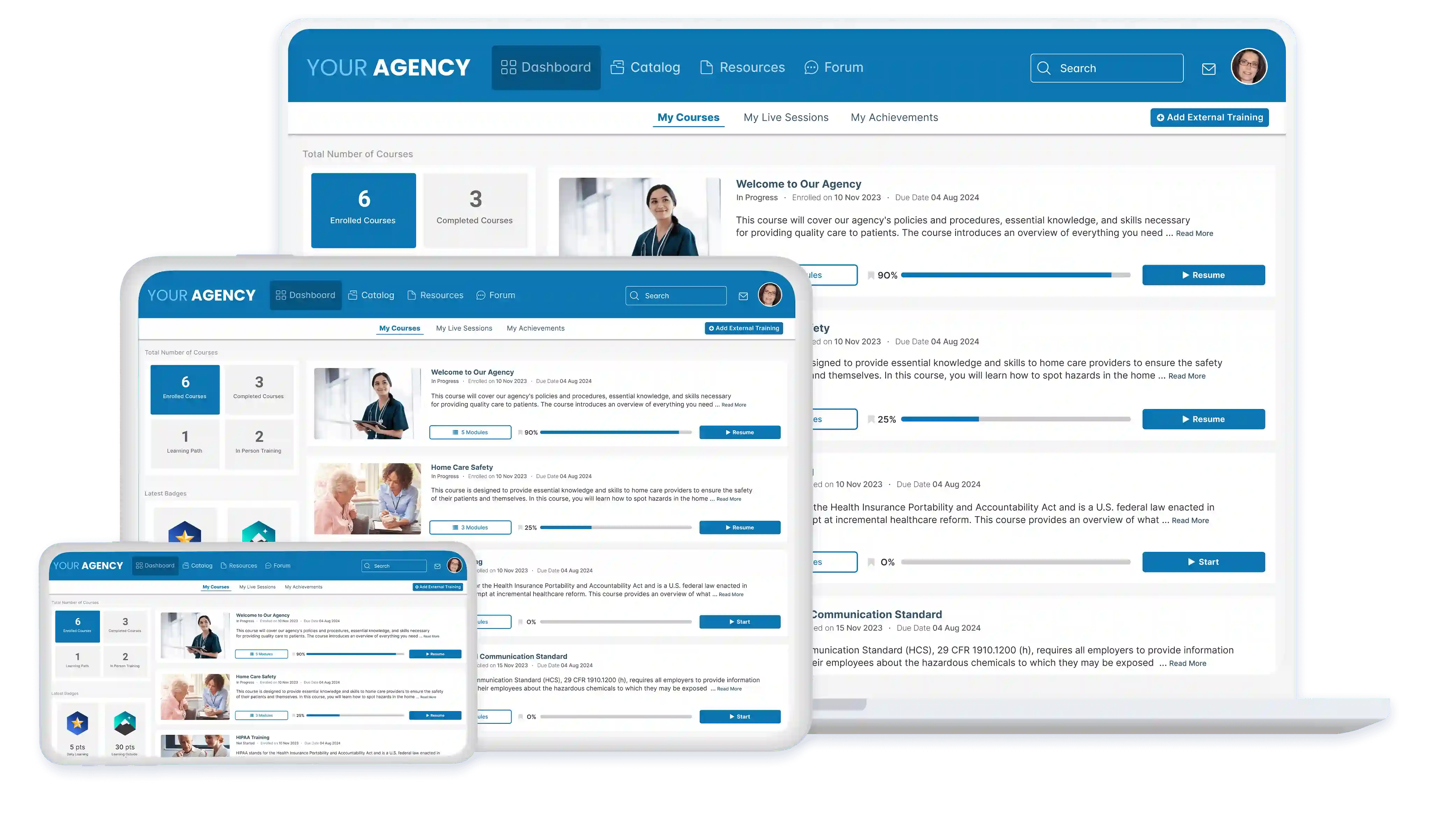
Best-in-class Home Care Learning Management System
Easy to customize, powerful at scale, and loaded with features and integrations for better care outcomes.
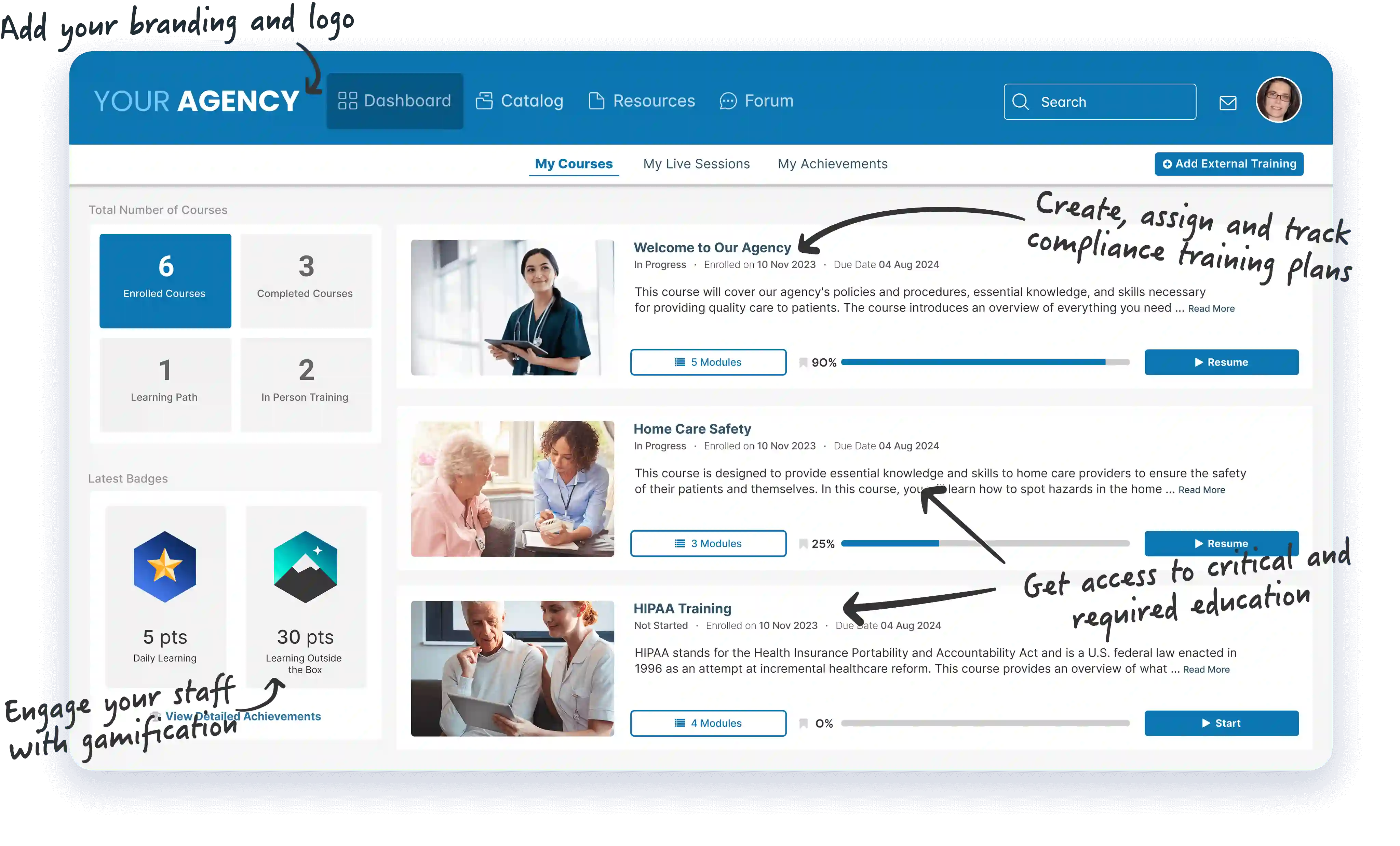
MOBILE FIRST EXPERIENCE
Home health training from anywhere, on any device
Say goodbye to a clunky learning experience. Home care, home health, and hospice staff are always on the go. Our platform is 100% mobile compatible on any modern phone, tablet or computer.
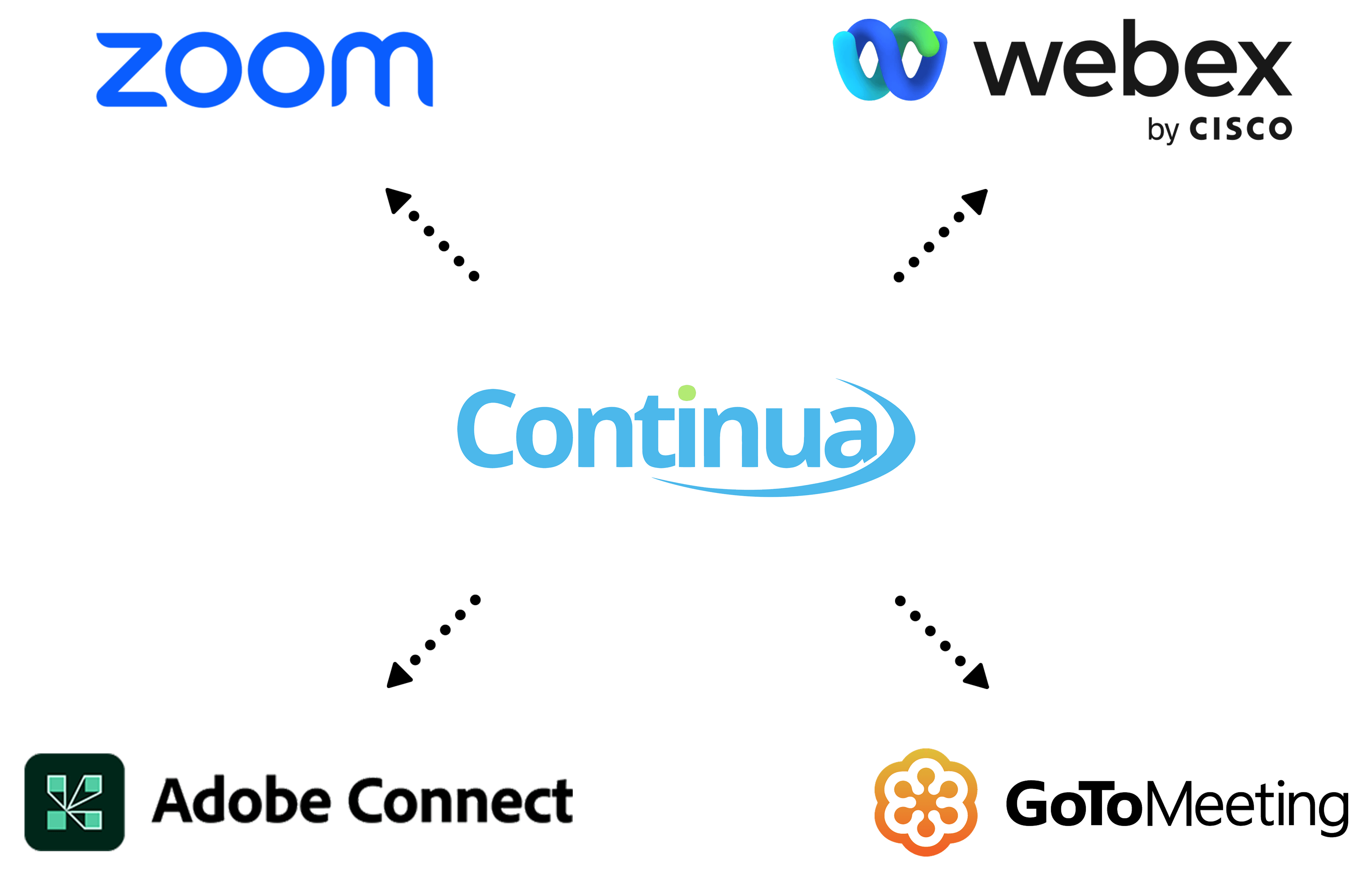
BLENDED HOME HEALTH TRAINING
Take your unique classroom instruction online
Connect your favorite webinar tool to a powerful instructor-led training (ILT) platform. Create, schedule, manage, and track all of your live classes for a truly blended training experience.
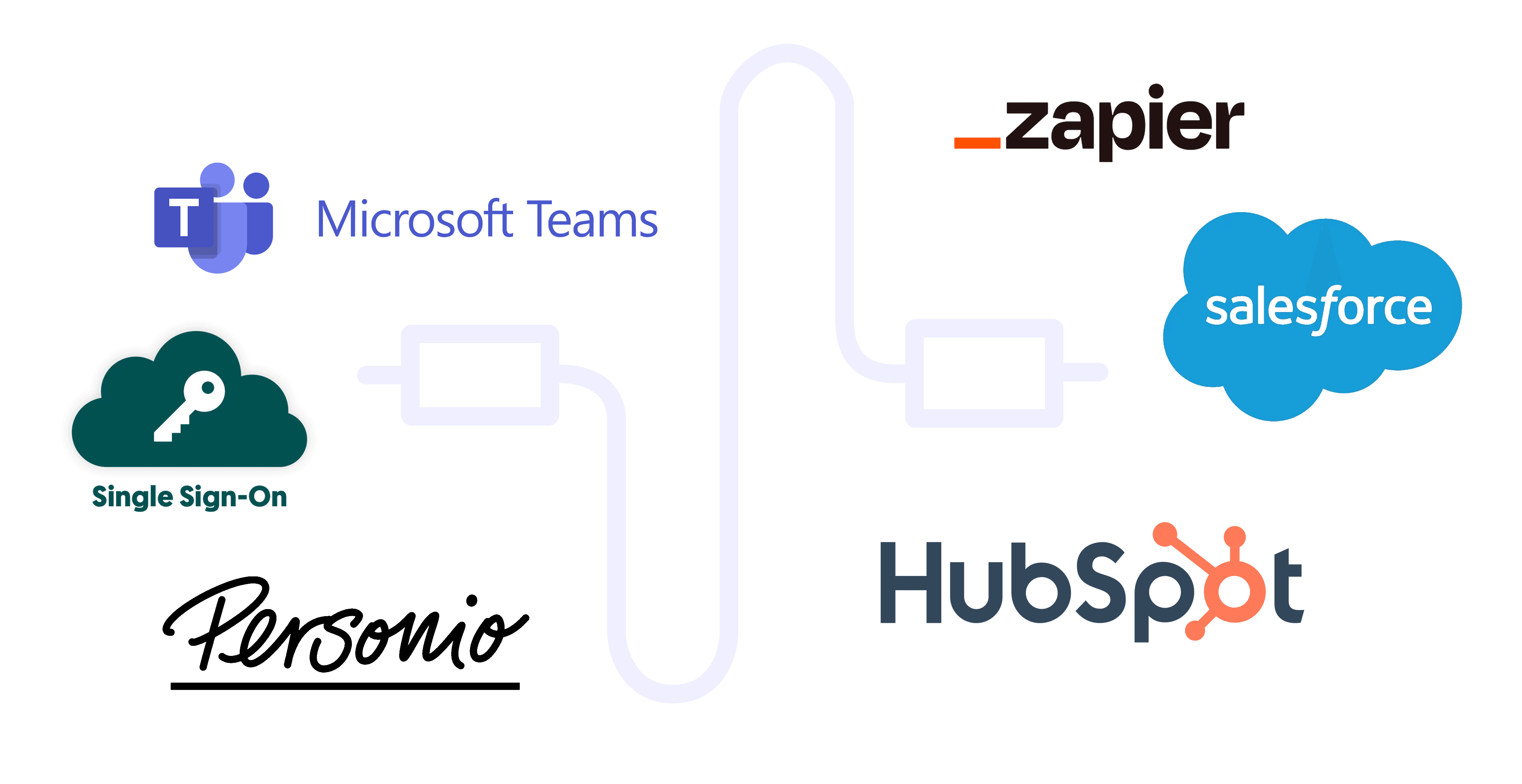
INTEGRATIONS
Seamlessly connect the tools you love
Make your tools work better together by integrating the software you already use with Continua Learning via a range of pre-built integrations or a robust API.
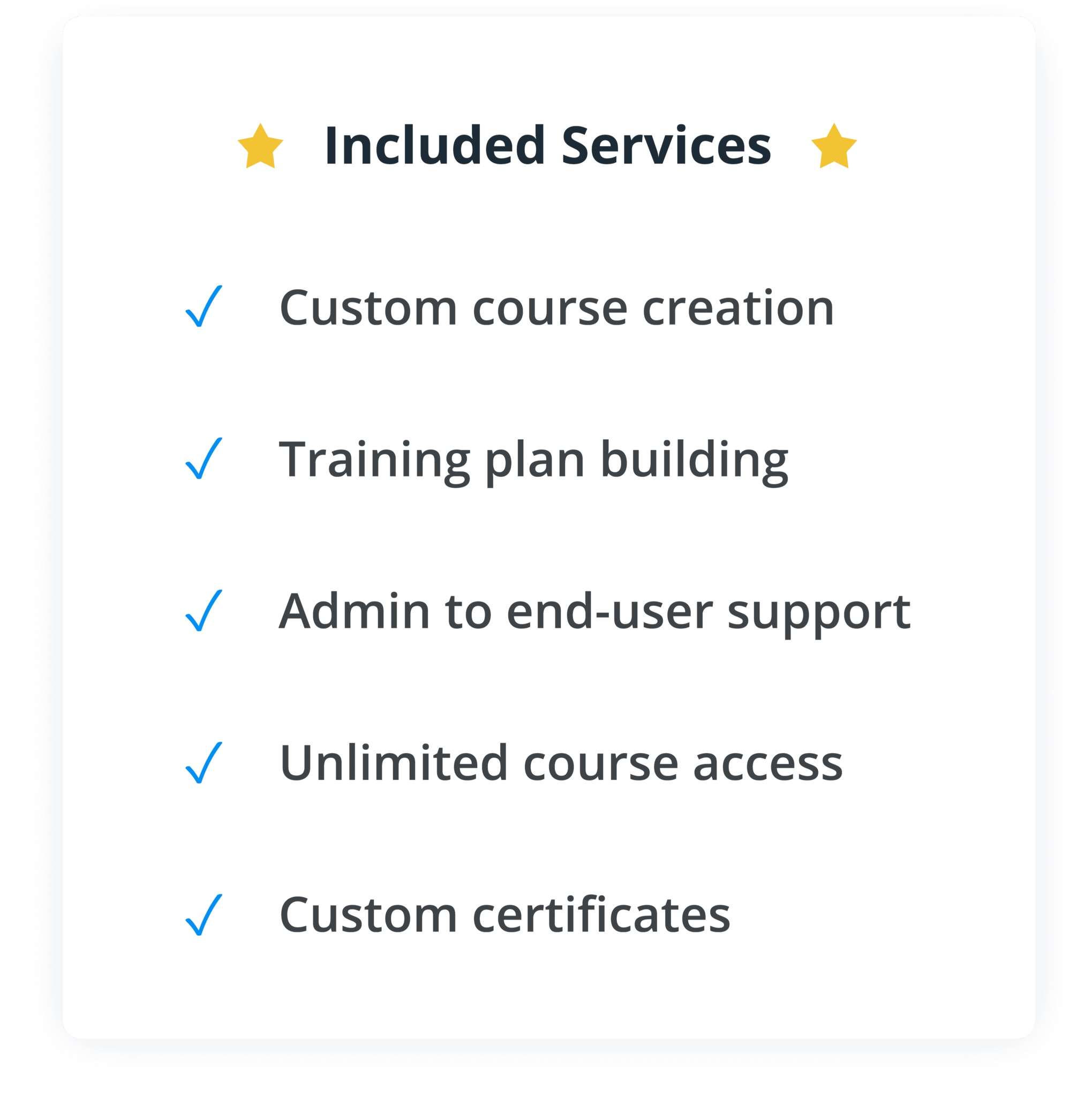
UNBEATABLE VALUE
Enjoy zero add-on costs
Don't get nickel and dimed by your training provider; with Continua Learning you get unlimited courses, services, and features at one cost-effective price.
Start Your Home Care Training Transformation Today
See why top care providers choose Continua Learning. Click below and complete the easy form to get a free demo with a training expert.
